Putting Patients &
Families First
Every year, millions of Americans living with serious illness struggle with untreated symptoms, fragmented care, and stress on families. Palliative care changes that. It provides an extra layer of support that improves quality of life, reduces unnecessary hospitalizations, and even lowers healthcare costs.
But access is uneven. The workforce is stretched thin. And too many patients never hear about palliative care until it’s too late. That’s where policy comes in.
Million
Expected Number of Americans Living with Serious Illness in the Next 25 Years
Our Policy Priorities
The Patient Quality of Life Coalition (PQLC) advances a consensus-based agenda to improve and expand access to high-quality palliative care. Our priorities focus on four key areas

Awareness & Education
Strengthen understanding among patients, families, and the public about the benefits of palliative care.

Workforce & Training
Expand and train healthcare professionals across disciplines to provide, teach, and sustain high-quality palliative care.

Research & Innovation
Build and invest in a robust evidence base that informs best practices and drives improvements in care delivery.

Access & Delivery
Ensure timely, equitable access to palliative care across hospitals, nursing homes, and community settings through better data, quality measurement, sustainable payment models, and appropriate access to essential medications.
Key Legislation
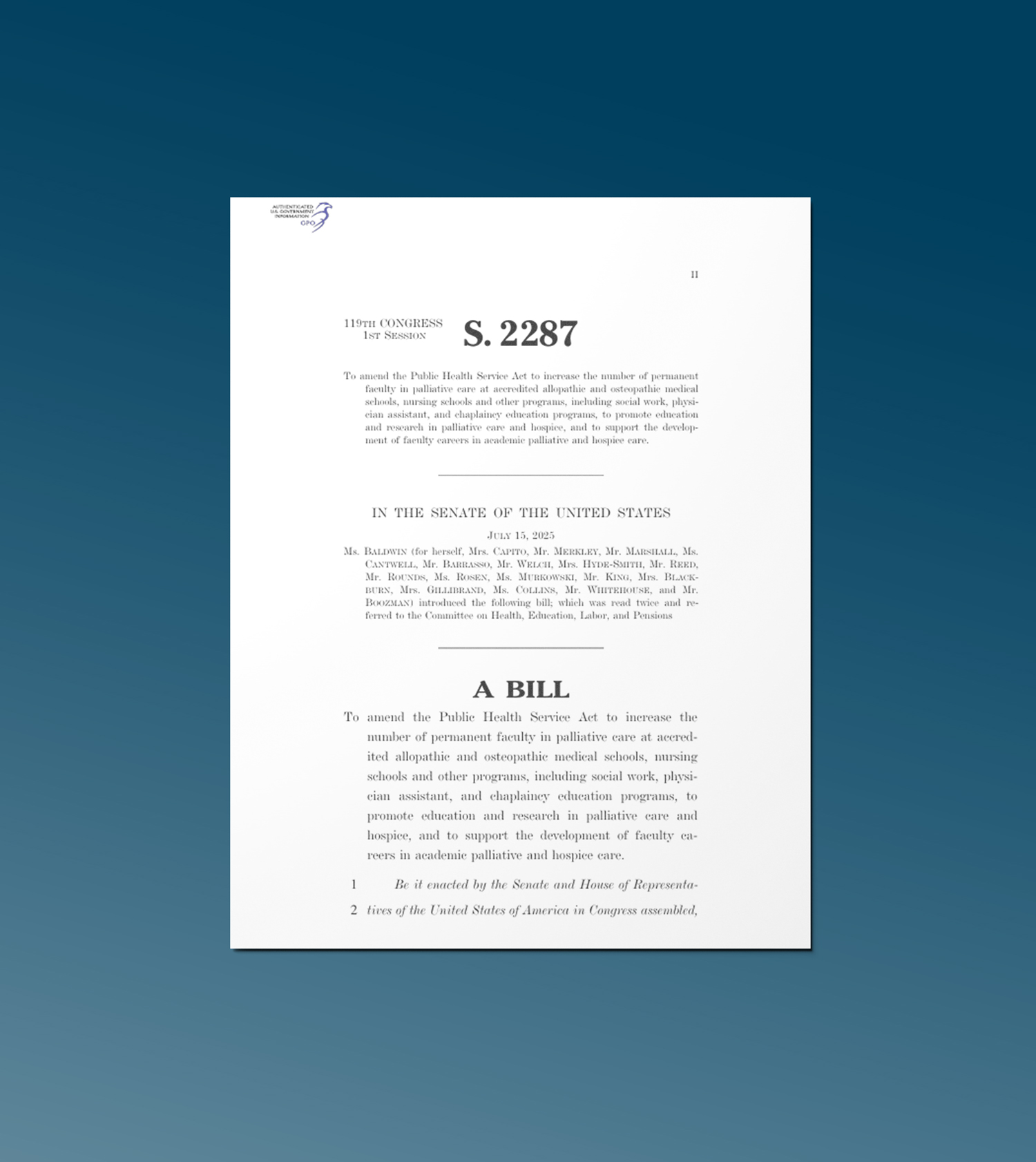
The Palliative Care and Hospice
Education and Training Act
PCHETA, S. 2287 & H.R. 4425
The Palliative Care and Hospice Education and Training Act
Bill Highlights
Education Programs
Create and expand training for interdisciplinary teams — physicians, nurses, social workers, physician assistants, chaplains, and more.
Physician Training
Provide grants to medical schools and teaching hospitals for rotations in palliative medicine across care settings.
Nurse Training
Expand opportunities in education, practice, and retention for hospice and palliative nursing.
Workforce Fellowships
Offer short-term intensive courses for faculty in medicine, nursing, psychology, pharmacy, social work, and chaplaincy.
Awareness Campaign
Launch a national campaign to inform patients, families, and providers about the benefits of palliative care.
Advocacy Efforts
PQLC continues to educate lawmakers, elevate patient and family voices, and build bipartisan support for policies that make palliative care accessible to all who need it.
How You Can Help
Spread the Word: Share resources about palliative care with your community.
Engage Policymakers: Urge your elected officials to support PCHETA.
PCHETA
Frequently Asked Questions
Question
Answer
What is the current status of PCHETA?
What are PCHETA’s key provisions?
PCHETA establishes interprofessional palliative care workforce training; launches a national palliative care education and awareness campaign; and enhances research in palliative care. For additional information, see the detailed bill summary.
Does PCHETA only focus on physicians?
No. PCHETA establishes programs to build palliative care capacity across all health care professions, including (but not limited to) physicians, nurses, social workers, physician assistants, chaplains, and others.
What is the status of palliative care in my state?
The Center to Advance Palliative Care (CAPC) issued a national scorecard that reviews each state’s capacity to deliver high-quality care to people facing serious illness.
Who supports PCHETA?
More than 50 national organizations and more than 50 state-based organizations. A full list of supporting organizations is available here.
Is PCHETA the same this (119th) Congress as previous Congresses?
- Yes, it is the same text as was introduced in the Senate in the 118th
- No substantive changes compared to the bill introduced in the Senate last (118th) Congress, the bill updates:
- Authorization years (i.e., “2024 to 2028” is changed to “2026 to 2030”)
- Required reporting date (i.e., “January 1, 2024” is changed to “January 1, 2026”)
- One section title
- Compared to PCHETA that passed the House in the 116th Congress the bill introduced in the 119th does the following:
- Further clarifies that palliative care shall not be furnished for the purpose of causing, or assisting in causing, a patient’s death
- Identical to bipartisan Senate language
- Supported by the U.S. Conference of Catholic Bishops
What does PCHETA cost?
The bill authorizes funds, subject to appropriation.
Has the Congressional Budget Office (CBO) scored this bill?
CBO reviewed the bill when the House passed PCHETA in a previous Congress.
If the appropriators provided the full amount authorized under the bill, it would cost up to $20 million per year for 5 years.